Post-Traumatic Stress Disorder (PTSD)
Traumatic events come in many forms. For some, trauma is losing a loved one or dealing with the pain of terminal illness. For many others, natural disasters and tragic events such as those in New Orleans and New York City or overseas in Paris or Israel have been life-altering. No matter the cause, these events can leave us feeling lost and helpless. If you have been diagnosed with Post-Traumatic Stress Disorder (PTSD), Dr. Diane® and her team can give you help and hope for a brighter future.
What is a Trauma vs. something being Traumatic?
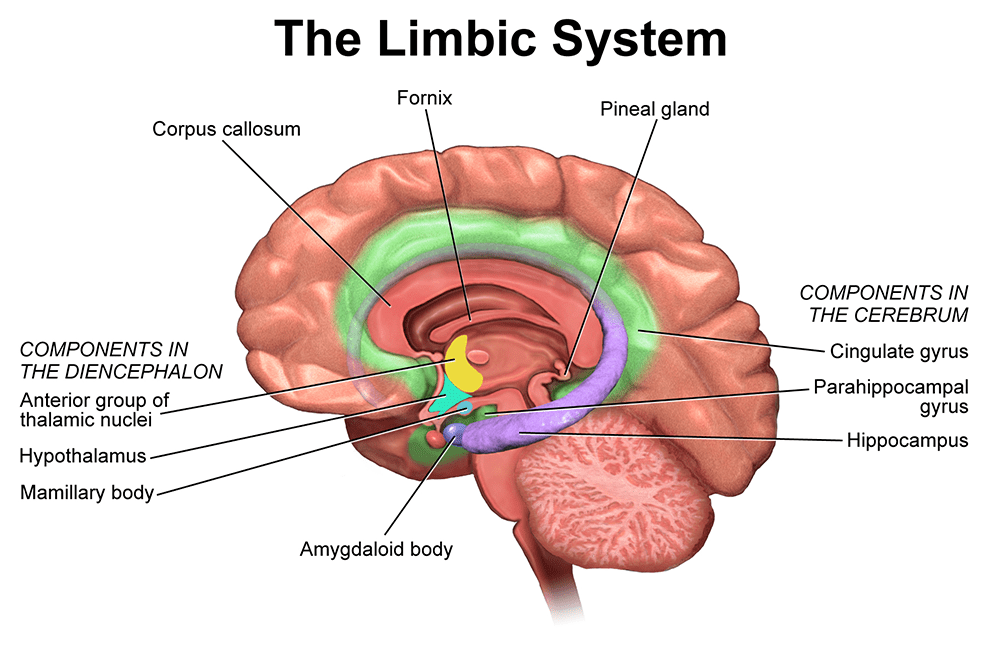
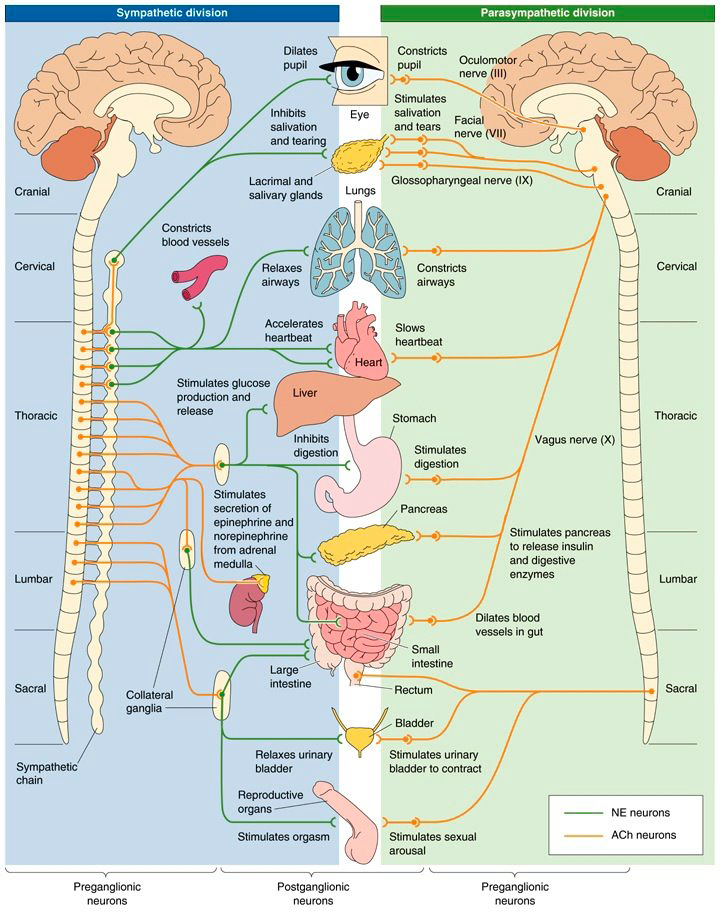
Post-Traumatic Stress Disorder (PTSD) is a psychological issue that happens when someone experiences a traumatic event that is not soothed or comforted. This lack of comfort activates the Amygdala, a tiny sensor in the middle of our brain, also called the limbic system. A person’s typical nervous system response is “fight or flight,” it sends a signal to our adrenal gland and vagus nerve, prompting us to react. PTSD results from trauma caused by combat, assault, domestic violence, and auto accidents.
When someone experiences a series of traumatic events, they can go on to suffer from Complex PTSD. The symptoms of Complex PTSD can be more enduring and extreme than those of PTSD. Many traumatic events happen for only a limited amount of time. In some cases, however, people experience chronic trauma that continues for months or years at a time. A PTSD diagnosis does not fully cover the severe psychological harm that occurs with prolonged trauma.
What is Trauma vs. something Traumatic?
When you experience something outside your typical life, your body and brain react in fear, a normal emotional response. A specific area of the brain controls your emotions like sadness, anger, and anxiety. This particular area is the limbic system also governs your autonomic response. The autonomic nervous system (ANS) automatically regulates body systems outside of voluntary control, such as heart rate and digestion.
Life experiences cause responses from both body and mind through our autonomic nervous system. Your body reacts without you putting any thought into it. If the situation feels life-threatening, your body goes into fight or flight mode. For example, if a lion is about to attack a goat, the goat senses this and starts to run away. In this situation, the brain sent a signal to the goat’s adrenal glands, creating a surge of adrenaline that enabled the goat to run.
The difference between trauma and traumatic experience is the ability to comfort and soothe the overstimulated limbic system. Fear in your everyday experience will likely have a support system that provides comfort, activating your frontal lobe. This part of the brain is the only part that thinks and responds. The rest of your brain is either for functional use or is reactive to protect itself. Suppose the brain sees an event as something to avoid yet feels emotionally in control. In that case, the adrenaline surge decreases, and the body becomes calm again. However, if there is repeated trauma without reasoning, the brain will continue to react in fear: fight or flight.
Trauma and Age
The age of a person who goes through trauma is important because the connection from the limbic system to the frontal lobe starts to develop at age three and finishes at age 24. This undeveloped connection is why infants cannot soothe themselves when they are afraid. It is also why children need parents or caregivers to bring reasoning and comfort. If a 5-year-old is scared, they run to one of their caregivers, who then hugs them and reassures them that they are safe. This comfort signals the reactive brain to calm down, but if this process does not happen, then the reactive brain continues signaling that the child is in danger.
PTSD and Memory
Flashbulb memory involves sights and sounds connected to an emotional event. For example, remembering a car accident while driving or hearing an airplane fly close to the city and recalling what you were doing on September 11, 2001, when you learned of the attacks on the Twin Towers. This type of memory is most common in Post-Traumatic Stress Disorder (PTSD) and is part of what is known as “flashbacks.”
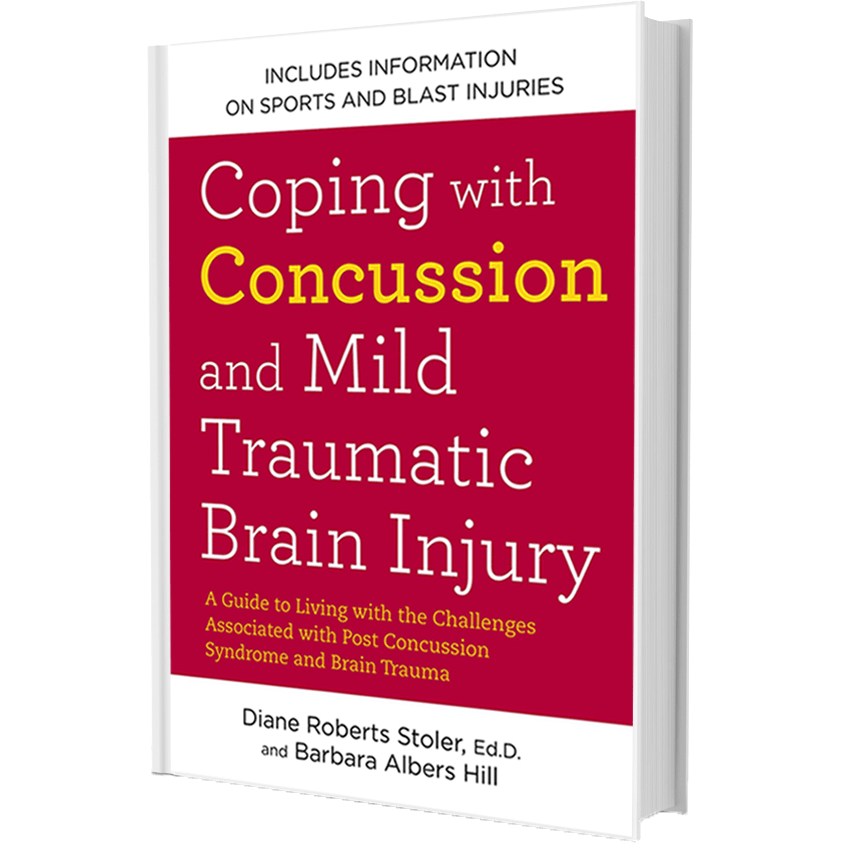
PTSD and Concussions
It should not surprise you to learn that psychological reactions come from the physical and emotional upheaval of a concussion, which is a traumatic brain injury from an outside force to the brain. A concussion causes dysregulations in the brain, making the brain unable to connect to the frontal lobe or recognize any comfort or soothing. Suppose you have a history of PTSD and have recently experienced a concussion. In that case, you will have heightened symptoms because there is a post-injury psychological reaction.
Why Post-Injury Psychological Reactions Occur
Similar to how your immune system kicks in as a response to a deep cut or an infection, the details and aftermath of brain trauma spark psychological responses. Physical and emotional pain that exceeds your threshold can make you feel nauseous or numb or even cause you to faint. Such physical reactions are often part of psychological upheaval.
What Are Some Elements of Post-Injury Psychological Reactions?
Psychological responses commonly involve emotional, cognitive, or behavioral elements. Emotional elements may include denial, avoidance, anxiety, emotional numbness, and feelings of grief or guilt. Cognitive reactions may take the form of rationalizing, blaming, or being judgmental. Behavioral elements may include aggressiveness, expressions of anger, withdrawal, lack of control, and extreme sadness. In many cases, behavioral responses develop into physical symptoms such as headaches, ulcers, chest pain, sleep problems. Extraordinary life experiences, including fire, assault, sports injury, car accidents, and combat, often lead to post-traumatic stress. The same is true of a concussion, either felt right away as acute stress or delayed response months or even years later.
What Post-Injury Psychological Reactions are Like
Post-concussive symptoms can feel like a personal disaster. You may have feelings of defeat, frustration, and inadequacy. In addition, you may suffer anxiety over your sudden lack of control over things and the sense that you have failed yourself and your family.
When your mind and body are neurologically dysregulated, your brain sends a distress signal to indicate that you are in danger. This signal may take the form of pain. Your mind or body’s reaction is to shut down through an initial response of numbness to avoid this pain. Following this shut-down phase is another response called the “fight-flight-freeze” mode.
Flight – Flight – Freeze Reactions
Some people react with the “fight” option. That is, they deal with aftereffects of an accident by showing verbal or physical aggression, angry outbursts, and blaming others. Others choose “flight;” where their reaction is to withdraw or flee. Flight happens in different ways, such as physical withdrawal (running from an accident scene) and denial (refusing to believe the event happened). Other ways are rationalization (coming up with an explanation for the accident) or guilt (blaming oneself). A person exhibits the “freeze” behavior by becoming so fearful that they become emotionally and/or physically paralyzed and unable to function.
Psychological responses will most likely be a mixture of reactions. Say you were in a car accident and got injured. Instead of focusing on your injuries or blaming yourself, it might be emotionally easier to blame the other driver. Especially if alcohol or drugs were involved, a loved one was injured, or if your injury resulted in a physical disability.
Symptoms by Type
- Amnesia – Yes
- Anger – Yes
- Lack of Awareness – Yes
- Concentration Problems – Yes
- Depression – Yes
- Despair – Yes
- Disorganization – Yes
- Distractibility – Yes
- Dizziness – Yes
- Lack of Emotion – Yes
- Fatigue – Yes
- Headaches – Yes
- Isolation and Withdrawal – Yes
- Poor Judgement – Yes
- Nightmares and Flashbacks – Yes
- Personality Changes – Yes
- Attempts to regain previous self-image – Yes
- Short-term Memory Loss – Yes
- Sleep Disturbances – Yes
- Ultimate acceptance/resolution – Yes
- Amnesia – Yes
- Anger – Yes
- Lack of Awareness – No
- Concentration Problems – Yes
- Depression – Sometimes
- Despair – Yes
- Disorganization – Yes
- Distractibility – Yes
- Dizziness – Sometimes
- Lack of Emotion – Yes
- Fatigue – Yes
- Headaches – Sometimes
- Isolation and Withdrawal – Yes
- Poor Judgement – No
- Nightmares and Flashbacks – Yes
- Personality Changes – Yes
- Attempts to regain previous self-image – Yes
- Short-term Memory Loss – Yes
- Sleep Disturbances – Yes
- Ultimate acceptance/resolution – Yes
- Amnesia – No
- Anger – Yes
- Lack of Awareness – No
- Concentration Problems – Yes
- Depression – Sometimes
- Despair – Yes
- Disorganization – Yes
- Distractibility – Yes
- Dizziness – Sometimes
- Lack of Emotion – No
- Fatigue – Yes
- Headaches – Sometimes
- Isolation and Withdrawal – Yes
- Poor Judgement – No
- Nightmares and Flashbacks – No
- Personality Changes – Sometimes
- Attempts to regain previous self-image – Yes
- Short-term Memory Loss – Sometimes
- Sleep Disturbances – Yes
- Ultimate acceptance/resolution – Yes